Why You Should Eat More Eggs in Winter 2024: The Science Behind the Super food
Diabetes 2024:Essential Authentic Knowledge Everyone Must Know!
Diabetes Mellitus
Diabetes mellitus, commonly known as diabetes, is a group of metabolic diseases characterized by high blood sugar levels over a prolonged period. This condition occurs when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces12.
Insulin is a hormone that regulates blood sugar. Hyperglycemia, or raised blood sugar, is a common effect of uncontrolled diabetes and, over time, leads to serious damage to many of the body’s systems, particularly the nerves and blood vessels2.
Types of Diabetes:
- Type 1 diabetes: Also known as insulin-dependent diabetes, it’s an autoimmune condition where the body’s immune system attacks and destroys the insulin-producing cells in the pancreas. People with type 1 diabetes require daily insulin injections to manage their blood sugar levels.
- Type 2 diabetes: This is the most common type and occurs when the body becomes resistant to insulin or doesn’t produce enough insulin. It’s often associated with obesity and a sedentary lifestyle, and it can sometimes be managed with lifestyle changes and medication.
- Gestational diabetes: This type occurs in some women during pregnancy and usually resolves after giving birth. However, it increases the risk of developing type 2 diabetes later in life.
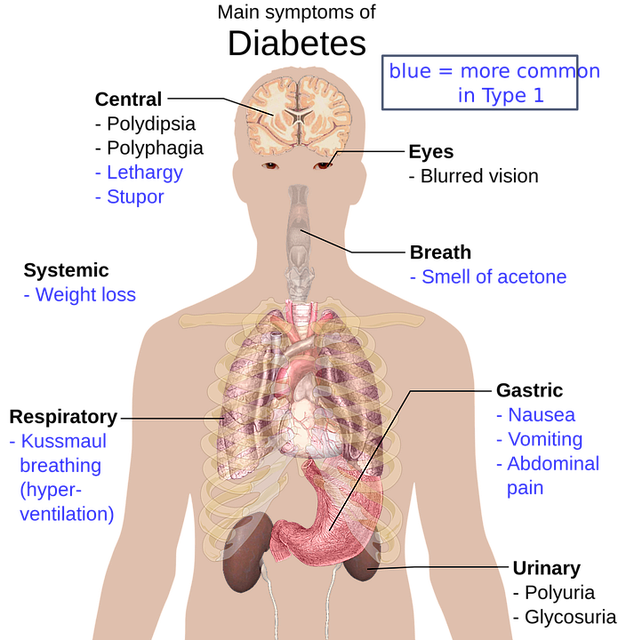
Symptoms of Diabetes:
can include increased thirst, frequent urination, hunger, fatigue, blurred vision, and unexplained weight loss. Long-term complications can include cardiovascular disease, stroke, chronic kidney disease, foot ulcers, and damage to the eyes2.
Managing diabetes involves monitoring blood sugar levels, following a healthy diet, regular physical activity, and using medication as prescribed. It’s also important for diabetics to have regular check-ups to monitor for potential complications12.
The causes of diabetes mellitus are multifactorial and differ depending on the type of diabetes:
- Type 1 diabetes is believed to be an autoimmune condition where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. The exact cause is not fully understood, but it is thought to involve a combination of genetic predisposition and environmental factors, such as exposure to certain viruses.
- Type 2 diabetes is primarily caused by lifestyle factors and genetics. Key contributors include being overweight or obese, leading a sedentary lifestyle, and having insulin resistance. Insulin resistance is a condition where muscle, liver, and fat cells do not use insulin effectively, which initially leads to an increased demand for insulin. Over time, the pancreas may fail to produce enough insulin to meet the body’s needs. Additionally, the distribution of body fat, particularly if more fat is stored around the abdomen, can increase the risk of type 2 diabetes1.
- Gestational diabetes occurs during pregnancy and is caused by hormonal changes that make the body’s cells less responsive to insulin. It can also be influenced by genetic and environmental factors1.
Other forms of diabetes can be caused by specific genetic mutations, diseases of the pancreas, certain medications, and infections or other illnesses1.
It’s important to note that while genetics provide the underlying susceptibility to diabetes, environmental factors, and lifestyle choices play a significant role in triggering the onset of the disease. Managing risk factors like diet, exercise, and body weight can help prevent or delay the development of type 2 diabetes21.
The early signs of diabetes can vary depending on the type, but here are some common warning signs to watch out for:
- Frequent Urination: When blood sugar levels are high, the kidneys try to remove the excess sugar by filtering it out of the blood. This can lead to a person needing to urinate more frequently, particularly at night12.
- Increased Thirst: Frequent urination necessary to remove excess sugar from the blood can result in the body losing additional water. Over time, this can cause dehydration and make a person feel more thirsty than usual12.
- Frequent Hunger: People with diabetes often do not get enough energy from their food. Glucose, the body’s fuel, doesn’t move efficiently from the bloodstream into cells. As a result, individuals with type 2 diabetes may feel constantly hungry, regardless of recent meals12.
- Fatigue: Type 2 diabetes can impact energy levels, causing fatigue due to insufficient sugar moving from the bloodstream into the body’s cells12.
- Blurry Vision: Excess sugar in the blood can damage tiny blood vessels in the eyes, leading to blurry vision. High blood sugar levels can also cause swelling of the eye lens, which improves when blood sugar levels reduce12.
- Slow Healing of Cuts and Wounds: High sugar levels impair blood circulation and damage nerves, resulting in slow wound healing. This also increases the risk of infection12.
- Tingling, Numbness, or Pain in Hands or Feet: High blood sugar levels can affect blood circulation and damage nerves, leading to sensations of tingling, numbness, or pain in the hands and feet (a condition known as neuropathy)2.
Remember that early detection and management are crucial for better outcomes. If you experience any of these symptoms, consult a healthcare professional for proper evaluation and guidance12.
Diabetes is diagnosed using several blood tests, which can determine if your blood glucose levels are within a healthy range. Here are the common tests used for diagnosing diabetes:
- A1C Test: This test measures your average blood sugar level over the past 2 to 3 months. An A1C level of 5% or higher on two separate tests indicates diabetes. A level between 5.7% and 6.4% suggests prediabetes, and below 5.7% is considered normal1.
- Fasting Blood Sugar Test: After fasting overnight, a blood sample is taken. A fasting blood sugar level of less than 100 mg/dL (5.6 mmol/L) is normal. A level from 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is considered prediabetes. If it’s 126 mg/dL (7 mmol/L) or higher on two separate tests, you have diabetes1.
- Glucose Tolerance Test: For this test, you fast overnight, and your fasting blood sugar level is measured. Then you drink a sugary liquid, and blood sugar levels are tested periodically for the next two hours. A blood sugar level of less than 140 mg/dL (7.8 mmol/L) is normal. A reading of more than 200 mg/dL (11.1 mmol/L) after two hours indicates diabetes. A reading between 140 and 199 mg/dL (7.8 mmol/L and 11.0 mmol/L) indicates prediabetes1.
- Random Blood Sugar Test: A blood sample is taken at a random time. Regardless of when you last ate, a blood sugar level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes1.
If your doctor suspects type 1 diabetes, they may also test your urine for the presence of ketones, which are substances made when the body breaks down fat for energy and can indicate type 1 diabetes1.
It’s important not to self-diagnose using over-the-counter blood testing equipment, as these cannot diagnose diabetes. If you suspect you might have diabetes or if you have risk factors for the disease, it’s crucial to see a healthcare professional for proper testing and diagnosis2.
The risk factors for developing diabetes can vary depending on the type:
- Type 1 Diabetes:
- Family History: Having a parent, brother, or sister with type 1 diabetes.
- Age: Although type 1 diabetes can occur at any age, it usually develops in children, teens, or young adults.
- Ethnicity: In the United States, White people are more likely to develop type 1 diabetes than African American and Hispanic or Latino people. However, currently, there is no known way to prevent type 1 diabetes1.
- Type 2 Diabetes:
- Prediabetes: If you have prediabetes (impaired glucose tolerance or impaired fasting glucose), you are at risk for type 2 diabetes.
- Weight: Being overweight increases the risk.
- Age: Being 45 years or older is a risk factor.
- Family History: Having a parent, brother, or sister with type 2 diabetes.
- Physical Activity: Being physically active less than 3 times a week.
- Gestational Diabetes: If you’ve ever had gestational diabetes during pregnancy or given birth to a baby who weighed over 9 pounds, you’re at risk.
- Ethnicity: African American, Hispanic or Latino, American Indian, or Alaska Native individuals are at higher risk. Some Pacific Islanders and Asian American people are also at risk.
- Non-Alcoholic Fatty Liver Disease: Having this condition may increase your risk for type 2 diabetes.
- Lifestyle Changes: Proven lifestyle changes, such as losing weight if you’re overweight, eating a healthy diet, and getting regular physical activity, can help prevent or delay type 2 diabetes1.
- Prediabetes:
- Similar to type 2 diabetes, the risk factors for prediabetes include being overweight, being 45 years or older, having a family history of type 2 diabetes, being physically inactive, and having a history of gestational diabetes.
- Lifestyle changes can prevent or reverse prediabetes1.
- Gestational Diabetes:
- Risk factors for gestational diabetes (diabetes during pregnancy) include:
- Having had gestational diabetes during a previous pregnancy.
- Giving birth to a baby who weighed over 9 pounds.
- Being overweight.
- Being more than 25 years old.
- Having a family history of type 2 diabetes.
- Having polycystic ovary syndrome (PCOS).
- Ethnicity: African American, Hispanic or Latino, American Indian, Alaska Native, Native Hawaiian, or Pacific Islander individuals.
- Gestational diabetes usually goes away after giving birth but increases the risk for type 2 diabetes. Babies born to mothers with gestational diabetes are more likely to have obesity as children or teens and may develop type 2 diabetes later in life1.
- Risk factors for gestational diabetes (diabetes during pregnancy) include:
Remember that early detection, lifestyle modifications, and regular check-ups are essential for managing diabetes risk.
Diabetes mellitus refers to a group of diseases that affect how the body uses blood sugar (glucose). Glucose is an important source of energy for the cells that make up the muscles and tissues. Let’s explore the major complications associated with diabetes:
- Eye Problems (Retinopathy):
- Diabetic retinopathy can affect eyesight. Regular eye screenings can detect it early, allowing for timely treatment and prevention of sight loss.
- Foot Problems:
- Diabetes-related foot problems are serious and can lead to amputation if left untreated.
- Nerve damage affects the feeling in your feet, and high blood sugar impairs circulation, making it slower for sores and cuts to heal.
- Notify your GP if you notice any changes in how your feet look or feel.
- Heart Attack and Stroke:
- High blood sugar damages blood vessels over time, increasing the risk of heart attacks and strokes.
- Kidney Problems (Nephropathy):
- Diabetes can damage the kidneys, making it harder to clear extra fluid and waste from the body.
- Known as diabetic nephropathy or kidney disease.
- Nerve Damage (Neuropathy):
- Complications of high blood sugar levels can cause nerve damage.
- Nerves may struggle to carry messages between the brain and the body, affecting vision, hearing, sensation, and movement.
- Gum Disease and Other Mouth Problems:
- Excess sugar in the blood can lead to more sugar in saliva, promoting bacterial growth.
- Acid produced by bacteria attacks tooth enamel and damages gums.
- Damaged blood vessels in the gums increase infection risk.
- Related Conditions, Like Cancer:
- People with diabetes are at higher risk of certain cancers.
- Some cancer treatments can impact diabetes control.
- Sexual Problems:
- In women, blood vessels and nerve damage can restrict blood flow to sexual organs, affecting sensation.
- Men may experience difficulty getting aroused or erectile dysfunction.
Remember, managing diabetes well, maintaining a healthy lifestyle, and attending regular appointments are essential for preventing or delaying these complications. 123
Managing blood sugar levels effectively is crucial for people with diabetes to prevent complications and maintain overall health. Here are some strategies to help you manage your blood sugar levels:
- Monitor Your Blood Sugar Regularly: Keep track of your blood sugar levels to understand how different foods, activities, and other factors affect them. Use a blood glucose meter or a continuous glucose monitor (CGM) as recommended by your healthcare provider1.

- Manage Your Diet:
- Control Carbohydrate Intake: Carbohydrates have the most significant impact on blood sugar levels. Learn to identify and manage the amount of carbs in your meals2.

- Choose Foods with a Low Glycemic Index: Foods with a low glycemic index (GI) raise blood sugar levels more slowly than high-GI foods2.
- Eat More Fiber: Fiber helps slow down the digestion of carbohydrates and the absorption of sugar, which can improve blood sugar control2.
- Control Carbohydrate Intake: Carbohydrates have the most significant impact on blood sugar levels. Learn to identify and manage the amount of carbs in your meals2.
- Exercise Regularly: Physical activity increases insulin sensitivity and helps your muscles use glucose effectively. Aim for a mix of aerobic exercises, resistance training, and flexibility exercises2.
- Stay Hydrated: Drinking enough water can help keep your blood sugar levels within healthy limits and prevent dehydration2.
- Implement Portion Control: Eating too much at one time can lead to higher blood sugar levels. Use measuring tools or visual cues to ensure appropriate portion sizes.
- Manage Stress: Stress can affect blood sugar levels, so it’s important to find ways to reduce stress, such as through meditation, yoga, or other relaxation techniques2.
- Get Enough Quality Sleep: Poor sleeping habits and a lack of rest can affect blood sugar levels
and insulin sensitivity. They can also increase appetite and promote weight gain2.
- Take Medications as Prescribed: If you’re on medications or insulin, take them as directed by your healthcare provider to help manage your blood sugar levels1.
- Plan Ahead: Have a plan for meals, physical activity, and medication. This can help you maintain more stable blood sugar levels throughout the day.
- Educate Yourself: Understanding diabetes and how it affects your body can help you make informed decisions about your health.
Remember, these are general guidelines, and it’s essential to work with your healthcare provider to create a personalized plan that fits your specific needs. They can provide you with detailed advice on monitoring your blood sugar, making dietary changes, and managing your condition effectively312.
Choosing the right snacks is essential for managing blood sugar levels effectively. Here are some diabetes-friendly snacks that are high in fibre, protein, and healthy fats:
- Hard-Boiled Eggs:
- Rich in protein, hard-boiled eggs help prevent blood sugar spikes.
- Enjoy them on their own or with a healthy topping like guacamole1.
- Yoghurt with Berries:
- Berries provide antioxidants that may reduce inflammation and support pancreas health.
- Yoghurt, especially Greek yogurt, helps lower blood sugar levels and adds protein1.
- Handful of Almonds:
- Almonds are nutritious and convenient.
- They contain vitamins, minerals, and healthy fats that can help control blood sugar1.
- Apple Slices with Nut Butter:
- Cottage Cheese:
- Vegetable Sticks with Hummus:
- Hummus is a great source of protein and fibre.
- Pair it with carrot, celery, or cucumber sticks for a satisfying snack2.
- Chia Pudding:
- Chia seeds are rich in fibre and protein.
- Mix them with unsweetened almond milk and let them soak to create a delicious pudding2.
- Air-Popped Popcorn:
- A whole-grain snack that provides fibre.
- Keep it plain or sprinkle with a dash of cinnamon for flavor3.
Remember to check your blood sugar levels before and after trying new foods to understand how they affect you personally. Enjoy these snacks while keeping portion sizes in mind! 123
Delicious and nutritious low-carb snack ideas that you can enjoy while keeping your carbohydrate intake in check:
- Olive Tapenade with Low-Carb Crackers:
- The Olive tapenade consists of chopped olives, capers, and olive oil. Olives are an excellent low-carb source of vitamin E, which functions as a powerful antioxidant in your body.
- Pair it with a low-carb cracker made from almond flour or seeds for a crunchy snack1.
- Homemade Trail Mix:
- Make a low-carb version by combining a variety of nuts and seeds, along with other low-carb ingredients like unsweetened coconut.
- For an easy trail mix recipe, combine pecan halves, chopped walnuts, roasted pumpkin seeds, and unsweetened coconut flakes1.
- Cheddar Cheese Crisps:
- Cheddar cheese is a versatile low-carb snack containing less than 1 gram of carbs per 1-ounce serving.
- Try homemade cheddar cheese crisps by baking thin slices of cheddar cheese until crisp, or look for packaged cheese crisps at the store.
- Deviled Eggs:
- Eggs are rich in vitamin B12 and choline, essential nutrients for brain health.
- Make deviled eggs by scooping out the egg yolks, and combining them with mayonnaise, Dijon mustard, salt, and pepper1.
- Celery Stuffed with Cream Cheese:
- Spread cream cheese into celery stalks for a crunchy and satisfying low-carb snack.
- Cucumber “Boats” Filled with Tuna Salad:
- Hollow out cucumber slices and fill them with tuna salad for a refreshing and protein-packed snack.
- Blackberries, Strawberries, or Raspberries:
- These fibre-rich berries are low in carbs and high in antioxidants.
- Pair them with a dollop of unsweetened whipped cream for a treat.
- Sliced Avocado:
- Avocado is a nutrient-dense fruit with healthy fats and fibre.
- Sprinkle it with salt and pepper or add a dash of lime juice for extra flavour.
Remember to choose snacks that align with your personal preferences and dietary needs. Enjoy these low-carb options!12
Insulin Resistance
Insulin resistance is a condition where the cells in your body don’t respond effectively to insulin, a hormone produced by the pancreas that helps regulate blood sugar levels. When you have insulin resistance, your muscle, fat, and liver cells can’t easily take up glucose from your blood, which can lead to higher blood sugar levels12.
How insulin resistance develops and its implications:
- Normal Insulin Function:
- Normally, when you eat, your body breaks down food into glucose, which enters your bloodstream.
- This increase in blood glucose signals your pancreas to release insulin.
- Insulin acts like a key, allowing glucose to enter your cells to be used for energy or stored for later use.
- As glucose enters your cells, blood sugar levels drop, signalling your pancreas to reduce insulin production.
- Development of Insulin Resistance:
- In insulin resistance, your cells don’t respond well to insulin’s “key,” and glucose struggles to enter your cells.
- This leads to higher levels of both glucose and insulin in your blood as your pancreas tries to compensate by producing more insulin.
- Over time, this can exhaust the pancreas, and it may not be able to produce enough insulin, leading to prediabetes and eventually type 2 diabetes if not managed properly.
- Associated Conditions:
- Symptoms and Diagnosis:
- Insulin resistance often has no symptoms initially. It’s usually identified through blood tests that measure blood sugar levels.
- Some signs that may indicate insulin resistance include a large waistline, high blood pressure, elevated fasting glucose levels, high triglycerides, low HDL cholesterol, skin tags, and patches of dark, velvety skin known as acanthosis nigricans2.
- Management and Prevention:
- Lifestyle changes are key in managing insulin resistance. This includes maintaining a healthy weight, engaging in regular physical activity, and eating a balanced diet rich in fibre and low in refined carbohydrates.
- Medications may also be prescribed to help improve insulin sensitivity and manage blood sugar levels.
Understanding and managing insulin resistance is crucial because it can significantly increase the risk of developing type 2 diabetes and other related health issues. If you suspect you might have insulin resistance, it’s important to consult a healthcare provider for proper evaluation and guidance12.
Improving insulin sensitivity is a key factor in managing diabetes and reducing the risk of developing type 2 diabetes. Here are some evidence-based strategies to enhance your insulin sensitivity:
- Exercise Regularly: Engaging in both aerobic and resistance training exercises can help increase insulin sensitivity. Aim for at least 30 minutes of moderate to vigorous activity most days of the week12.
- Maintain a Healthy Weight: Weight loss, particularly reducing belly fat, can significantly improve insulin sensitivity1.
- Eat a Balanced Diet:
- Increase Fiber Intake: Foods high in soluble fibre, such as fruits, vegetables, legumes, and whole grains, can improve insulin sensitivity1.
- Include Foods Rich in Omega-3 Fatty Acids: Such as fish, flaxseeds, and walnuts1.
- Limit Sugars and Refined Carbs: Reducing intake of high-glycemic foods can help manage blood sugar levels1.
- Get Adequate Sleep: Lack of sleep can lead to reduced insulin sensitivity. Aim for 7-9 hours of quality sleep per night.
- Manage Stress: Chronic stress can impair insulin sensitivity. Techniques like meditation, yoga, and deep breathing exercises can help manage stress levels.
- Stay Hydrated: Drinking plenty of water throughout the day can help maintain normal blood sugar levels1.
- Limit Alcohol Intake: Excessive alcohol can negatively affect insulin sensitivity, so it’s best to consume it in moderation1.
- Consider Supplements: Some supplements, like magnesium and chromium, may improve insulin sensitivity. However, always consult with a healthcare provider before starting any new supplement1.
- Avoid Sedentary Behaviors: Break up long periods of sitting with short activity breaks to help improve insulin sensitivity1.
- Monitor Your Blood Sugar Levels: Keeping track of your blood sugar can help you understand how different foods and activities affect your insulin sensitivity1.
Moringa, often available in capsule form, has been studied for its potential health benefits, including its effects on blood sugar levels. Research suggests that Moringa oleifera, also known as the drumstick tree, may have several health benefits due to its antioxidant and anti-inflammatory properties1


Specifically for diabetes, some studies indicate that Moringa may help lower blood sugar levels. It contains compounds like quercetin, which can increase glucose uptake by muscles and reduce glucose production in the liver, and chlorogenic acid, which may slow down glucose absorption in the intestines2. Additionally, insulin-like proteins found in Moringa might help improve how the body processes sugar, and it may affect insulin release3.
While Moringa may not cure diabetes completely, it could potentially reduce the likelihood of diabetes by lowering blood sugar and improving insulin resistance. It’s also noted for providing an energy boost, which can be beneficial as people with diabetes can easily become tired due to the body’s excessive urine and water loss.
However, it’s important to approach the use of Moringa with caution, especially if you are already on medication for diabetes, as it may interact with your treatment plan. Always consult with a healthcare provider before adding any new supplement to your regimen to ensure it’s safe and appropriate for your specific health needs1234.
Disclaimer: The contents of this article are intended to raise awareness about common health issues and should not be viewed as sound medical advice for your specific condition. You should always consult with a licensed medical practitioner before following any suggestions outlined in this article or adopting any treatment protocol based on the article’s contents.
If you enjoyed this article, please like and share it with your friends, and don’t forget to subscribe for more great content!
Human Traits: Cultivating Positive Traits and Overcoming Negative Ones

