Monkeypox
Simple Explanation of Monkeypox:
What is Monkeypox?
- Monkeypox is a disease caused by a virus.
- It can make you feel sick and give you a rash.
How Do You Get It?
- From Animals: You can get it by touching animals that have the virus, like certain rodents.
- From People: You can also get it by touching someone who is sick with monkeypox or their clothes and bedding.
What Are the Symptoms?
- Fever: You might feel very hot.
- Headache: Your head might hurt.
- Muscle Aches: Your body might feel sore.
- Rash: You get red spots on your skin that turn into blisters.

The backs of the hands of a patient with monkeypox show a characteristic rash during his recovery phase. Monkeypox outbreak in the Democratic Republic of the Congo (DRC), 1996-1997, formerly in Zaire. In 1996, 71 suspected cases of human monkeypox were reported in Katako-Kombe. In February 1997 epidemiological observations and laboratory results led to the conclusion that the repeated reintroduction of monkeypox virus by animals is necessary to maintain the disease in the local human population. (Photo by: CDC/IMAGE POINT FR/BSIP/Universal Images Group via Getty Images)
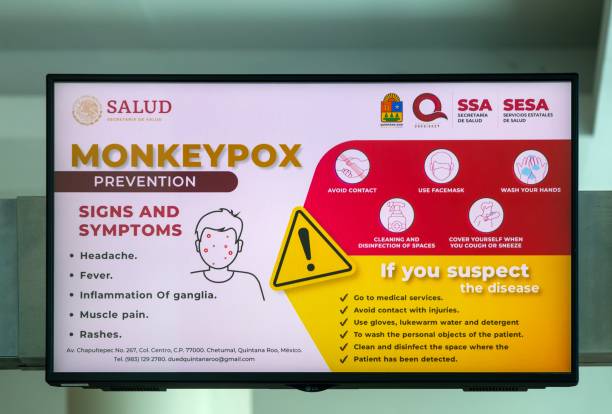
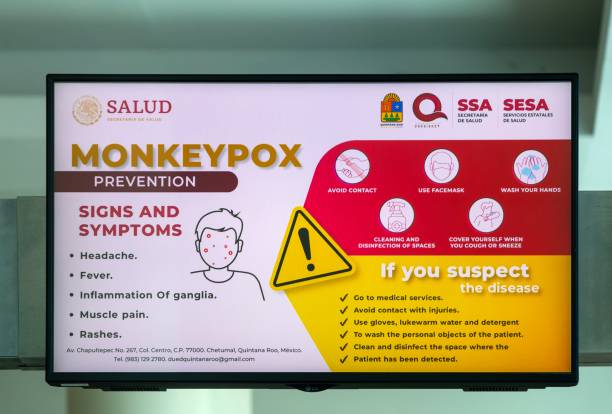
How to Stay Safe?
- Avoid Touching: Don’t touch animals or people who are sick.
- Wash Hands: Keep your hands clean by washing them often.
- Use Protection: Wear gloves and masks if you are caring for someone who is sick.
What to Do If You Feel Sick?
- See a Doctor: Go to a health clinic or hospital.
- Stay Away from Others: Try not to be close to other people to avoid spreading the virus.
Smallpox and Monkeypox are Both Viral Diseases Caused by Viruses from the Orthopoxvirus Family, but They Have Some Key Differences:
Smallpox
- Causative Agent: Variola virus.
- Symptoms: High fever, fatigue, severe headache, backache, and a characteristic rash that progresses to pus-filled sores.
- Transmission: Highly contagious, spread through respiratory droplets, direct contact with infected bodily fluids, or contaminated objects.
- Severity: Historically, smallpox had a high mortality rate and caused severe illness.
- Lymphadenopathy: Does not cause swelling of the lymph nodes.
- Eradication: Declared eradicated in 1980 after a successful global vaccination campaign1.
Monkeypox
- Causative Agent: Monkeypox virus.
- Symptoms: Fever, headache, muscle aches, backache, swollen lymph nodes, chills, and a rash that often begins on the face and spreads to other parts of the body.
- Transmission: Less contagious than smallpox, spread through close contact with infected animals or humans, and respiratory droplets or contact with contaminated materials.
- Severity: Generally milder than smallpox, with a lower mortality rate, but can still cause serious illness.
- Lymphadenopathy: Causes noticeable swelling of the lymph nodes, which is a distinguishing feature from smallpox23.
Both diseases share some similarities in symptoms, but the presence of swollen lymph nodes in monkeypox and the higher severity and contagiousness of smallpox are key differences.
Monkeypox Has an Intriguing History, Marked by Several Significant Outbreaks and Discoveries:
Initial Discovery
1958: Monkeypox was first identified in laboratory monkeys in Copenhagen, Denmark, during two outbreaks of a pox-like disease12. Despite its name, the primary reservoirs of the virus are believed to be rodents, not monkeys1.
First Human Case
1970: The first human case of monkeypox was recorded in a 9-month-old boy in the Democratic Republic of the Congo (DRC)3. This occurred during intensified efforts to eradicate smallpox, which led to increased surveillance for pox-like illnesses3.
Subsequent Outbreaks
1980s-1990s: Sporadic cases and outbreaks were reported primarily in Central and West African countries, including the DRC, Nigeria, and Cameroon3.
2003: The first outbreak outside of Africa occurred in the United States, linked to imported African rodents that infected pet prairie dogs3. This outbreak resulted in over 70 cases but no fatalities3.
Recent Global Outbreak
2022-2023: A significant global outbreak began in May 2022, with cases reported in multiple non-endemic countries, including Europe and North America13. This outbreak was notable for its rapid spread and the involvement of the West African clade of the virus, which is less severe than the Central African clade3.
Monkeypox’s History Highlights the Importance of Global Surveillance and Preparedness to Manage Emerging Infectious Diseases.
The recent monkeypox outbreak began in early May 2022, with cases reported in countries where the disease is not typically found1. Most of these cases were linked to travel to Europe and North America, rather than the traditional endemic regions of West and Central Africa1.
Key Points:
- Initial Cases: The outbreak started with cases in non-endemic countries, primarily in Europe and North America1.
- Transmission: The virus spread through close contact, including sexual contact, and was identified mainly among men who have sex with men1.
- Strains: The outbreak involved the West African clade of the monkeypox virus, which is less severe compared to the Central African clade23.
Recent Developments:
- Central Africa: In 2024, a concerning strain of the monkeypox virus spread rapidly across Central Africa, prompting the Africa Centres for Disease Control and Prevention to declare a public health emergency4.
- Transmission: Monkeypox can spread through direct contact with infected animals or humans, respiratory droplets, and contaminated materials3.
- Symptoms: Include fever, headache, muscle aches, backache, swollen lymph nodes, chills, and a characteristic rash3.
- Prevention: Measures include avoiding contact with infected individuals or animals, practicing good hygiene, and vaccination3.
Monkeypox Symptoms Typically Appear Within 6 to 13 Days after Exposure, but This Can Range From 5 to 21 Days1. The Common Symptoms:
Early Symptoms
- Fever: Often the first symptom.
- Headache: Persistent and severe.
- Muscle Aches: General body pain.
- Backache: Specific pain in the back.
- Fatigue: Feeling very tired.
- Chills: Shivering and feeling cold.
- Swollen Lymph Nodes: Noticeable swelling, especially in the neck, armpits, or groin12.
Rash Development
- Initial Rash: Begins as flat, discoloured lesions (macules).
- Progression: Lesions evolve into raised bumps (papules), then fluid-filled blisters (vesicles), followed by pus-filled sores (pustules).
- Scabbing: Lesions eventually scab over and fall off12.
Rash Locations
- Face: Most common site.
- Palms and Soles: Hands and feet.
- Mouth: Inside the mouth.
- Genitalia: Around the genital area.
- Eyes: Including the conjunctivae and cornea1.
Duration
The Risk Factors for Monkeypox
Several factors can increase the risk of contracting monkeypox. Here are the main risk factors:
Close Contact with Infected Individuals
- Household Members: Living with someone who has monkeypox increases the risk of transmission1.
- Healthcare Workers: Due to their close contact with patients, healthcare workers are at higher risk2.
- Sexual Partners: Engaging in intimate contact with an infected person can lead to transmission2.
Exposure to Infected Animals

- Handling Animals: Direct contact with infected animals, such as rodents or primates, can transmit the virus1.
- Animal Bites or Scratches: Being bitten or scratched by an infected animal1.
- Consuming Infected Meat: Handling or eating undercooked meat from infected animals1.
Immunocompromised Individuals
- Weakened Immune Systems: People with compromised immune systems are at higher risk of severe disease3.
- Pregnant Women and Children: These groups are more susceptible to severe symptoms and complications3.
Living in or Traveling to Endemic Areas
- Endemic Regions: Living in or travelling to areas where monkeypox is endemic, such as parts of Central and West Africa2.
Occupational Exposure
Understanding these risk factors can help in taking preventive measures to reduce the likelihood of infection.
Diagnosing monkeypox involves several steps to confirm the presence of the virus. Here’s an overview of the diagnostic process:
Clinical Evaluation
- Medical History: Doctors review the patient’s medical history and assess possible exposures or risk factors, such as recent travel to endemic areas or contact with infected individuals1.
- Physical Examination: A thorough examination is conducted, focusing on the characteristic rash and other symptoms like fever, swollen lymph nodes, and muscle aches1.
Laboratory Testing
- Sample Collection: Samples are taken from skin lesions, including vesicles, pustules, or scabs. These samples are crucial for accurate diagnosis12.
- Polymerase Chain Reaction (PCR): The primary method for confirming monkeypox is PCR testing, which detects the DNA of the monkeypox virus in the collected samples23.
- Other Tests: In some cases, additional tests may be performed to rule out other infections with similar symptoms, such as herpes simplex virus, syphilis, or chickenpox1.
Differential Diagnosis
- Other Conditions: Doctors consider other possible causes of the symptoms, including other poxvirus infections, allergic reactions, and various skin conditions1.
Importance of Early Diagnosis
- Preventing Spread: Early and accurate diagnosis is essential to prevent the spread of the virus and to provide appropriate care to the infected individual1.
Monkeypox Can Lead to Several Complications, Some of Which Can Be Severe. The Main Complications Associated with Monkeypox:
Common Complications
- Secondary Infections: Bacterial infections of the skin lesions can occur, leading to further complications1.
- Bronchopneumonia: Infection of the lungs, which can cause breathing difficulties2.
- Sepsis: A life-threatening response to infection that can lead to tissue damage and organ failure2.
- Encephalitis: Inflammation of the brain, which can cause neurological symptoms and long-term damage2.
- Corneal Infection: Infection of the cornea, which can lead to vision loss2.
Other Potential Complications
- Severe Dehydration: Due to vomiting and diarrhoea, which can lead to malnutrition1.
- Painful Lesions: Lesions in sensitive areas such as the mouth, eyes, and genitalia can cause significant discomfort and complications1.
- Scarring: Permanent scarring from the skin lesions1.
Risk Factors for Severe Complications
- Immunocompromised Individuals: People with weakened immune systems are at higher risk of severe complications3.
- Children and Pregnant Women: These groups are more susceptible to severe symptoms and complications3.
Prevention and Management
- Early Diagnosis and Treatment: Prompt medical attention can help manage symptoms and prevent complications1.
- Vaccination: Vaccines developed for smallpox can also provide protection against monkeypox1.
Understanding these complications highlights the importance of preventive measures and early medical intervention.
Currently, no specific treatment is approved exclusively for monkeypox. However, several approaches can help manage the symptoms and prevent complications:
Supportive Care
- Symptom Relief: Pain relievers like ibuprofen or acetaminophen can help reduce fever and pain1.
- Hydration: Drinking plenty of fluids to stay hydrated and maintain electrolyte balance2.
- Skin Care: Keeping the rash clean and dry, and avoiding touching the lesions to prevent secondary infections1.
Antiviral Treatments
- Tecovirimat (TPOXX): An antiviral medication that has shown promise in treating monkeypox. It is available under an expanded access protocol for certain patients, such as those with severe disease or weakened immune systems3.
- Other Antivirals: Research is ongoing to determine the effectiveness of other antiviral drugs in treating monkeypox3.
Preventive Measures
- Isolation: Infected individuals should isolate themselves to prevent spreading the virus to others2.
- Vaccination: Vaccines developed for smallpox, such as the JYNNEOS vaccine, can also protect monkeypox3.
Management of Complications
- Secondary Infections: Antibiotics may be prescribed if bacterial infections develop in the skin lesions3.
- Severe Cases: Hospitalization may be required for severe cases, especially for those with complications like encephalitis or sepsis3.
Ongoing Research
- Clinical Trials: Studies are being conducted to evaluate the safety and efficacy of various treatments for monkeypox3.
Recovery From Monkeypox Typically Takes Between 2 to 4 Weeks. Here’s a Breakdown of the Recovery Process:
Initial Phase (1-2 Weeks)
- Early Symptoms: Fever, headache, muscle aches, and swollen lymph nodes appear first.
- Rash Development: The rash progresses through stages, starting as flat lesions, then raised bumps, fluid-filled blisters, and finally pus-filled sores.
Healing Phase (2-4 Weeks)
- Scabbing: The sores eventually scab over and begin to heal.
- Falling Off: Scabs fall off, leaving the skin underneath to heal completely.
Factors Influencing Recovery
- Severity of Infection: Milder cases may recover faster, while severe cases might take longer.
- Immune System: Individuals with strong immune systems tend to recover more quickly.
- Complications: The presence of complications like secondary infections can prolong recovery.
Post-Recovery
- Scarring: Some individuals may experience scarring where the lesions are.
- Fatigue: It’s common to feel fatigued even after the visible symptoms have resolved.
Monkeypox and COVID-19 differ significantly in terms of lethality and transmission potential:
Lethality
- Monkeypox: The fatality rate for monkeypox varies between 0% and 11%, depending on the strain and the population affected1. The recent outbreak in Africa has shown a fatality rate around 3%, with higher rates in certain vulnerable groups1.
- COVID-19: The fatality rate for COVID-19 has varied widely, influenced by factors such as age, underlying health conditions, and access to medical care. Globally, the case fatality rate has been estimated at around 1-2%, but it has been much higher in older adults and those with pre-existing conditions2.
Transmission
- Monkeypox: Primarily spreads through close skin-to-skin contact, respiratory droplets during prolonged face-to-face interaction, and contact with contaminated materials like bedding or clothing3. It does not spread as easily as COVID-19 and is less likely to cause widespread outbreaks3.
- COVID-19: Spreads mainly through respiratory droplets and aerosols, making it highly contagious, especially in crowded or poorly ventilated spaces2. Asymptomatic transmission has also played a significant role in its rapid global spread2.
Global Spread Potential
- Monkeypox: While monkeypox can spread internationally, its transmission dynamics make it less likely to cause a pandemic on the scale of COVID-193. The visible symptoms and slower transmission rate help in identifying and isolating cases more effectively4.
- COVID-19: The virus’s ability to spread quickly and silently, often before symptoms appear, contributed to its rapid global spread and pandemic status2.
In summary, while monkeypox can cause serious illness and has a higher fatality rate in certain populations, it is less likely to spread globally like COVID-19 due to its transmission characteristics.
Countries Vulnerable to Monkeypox Spread
Countries in Central and West Africa are traditionally more vulnerable to monkeypox due to the presence of the virus in local wildlife and the higher likelihood of human-animal interactions.
Countermeasures to Lessen the Spread
To reduce the chances of monkeypox spreading, several preventive measures can be implemented:
Public Health Measures
- Surveillance and Reporting: Strengthening disease surveillance systems to quickly identify and report cases3.
- Isolation and Quarantine: Isolating infected individuals and quarantining those who have been exposed3.
- Vaccination: Using vaccines like JYNNEOS for high-risk populations, including healthcare workers and those in outbreak areas3.
Personal Protective Measures
- Avoid Close Contact: Refrain from close physical contact with individuals showing symptoms of monkeypox3.
- Hygiene Practices: Regular hand washing with soap and water or using alcohol-based hand sanitizers3.
- Protective Clothing: Wearing gloves and protective clothing when handling animals or caring for infected individuals4.
Community Engagement
- Education and Awareness: Informing communities about the symptoms, transmission, and prevention of monkeypox3.
- Reducing Stigma: Encouraging supportive environments to reduce stigma and ensure that affected individuals seek medical care promptly3.
Environmental Measures
- Disinfection: Cleaning and disinfecting surfaces and materials that may have been contaminated by the virus3.
- Safe Animal Handling: Avoiding contact with wild animals, particularly rodents and primates, and ensuring safe handling and cooking of animal products4.
Implementing these measures can significantly reduce the risk of monkeypox spreading within and beyond vulnerable regions. If you have any more questions or need further details, feel free to ask!
The World Health Organization (WHO) has implemented several measures to educate the public about monkeypox and to prevent its spread. Here are some key initiatives:
Educational Measures
- Public Awareness Campaigns: WHO has launched campaigns to inform the public about monkeypox symptoms, transmission, and prevention. These campaigns use various media platforms to reach a wide audience1.
- Guidance for Healthcare Workers: Providing detailed guidelines and training for healthcare workers to identify, manage, and report monkeypox cases2.
- Community Engagement: Working with community leaders and organizations to spread awareness and educate people about preventive measures1.
Strategic Preparedness and Response Plan (SPRP)
WHO’s Monkeypox Strategic Preparedness, Readiness, and Response Plan outlines a comprehensive approach to manage the outbreak3. Key objectives include:
- Interrupting Human-to-Human Transmission: Implementing effective public health measures such as isolation, contact tracing, and vaccination3.
- Protecting Vulnerable Groups: Focusing on groups at higher risk, such as healthcare workers and immunocompromised individuals3.
- Minimizing Zoonotic Transmission: Reducing the risk of transmission from animals to humans through safe handling practices and public education3.
Preventive Measures
- Vaccination: Promoting the use of vaccines like JYNNEOS for high-risk populations4.
- Hygiene Practices: Encouraging regular hand washing, use of hand sanitizers, and avoiding contact with infected individuals or animals5.
- Isolation and Quarantine: Advising isolation of infected individuals and quarantine for those exposed to the virus5.
Research and Development
- Ongoing Research: Supporting research to better understand the virus, its transmission, and effective treatments3.
- Collaboration: Working with international partners to develop and distribute vaccines and treatments3.
Monitoring and Surveillance
- Enhanced Surveillance: Strengthening disease surveillance systems to quickly detect and respond to new cases2.
- Data Sharing: Facilitating the sharing of data and information between countries to track the spread of the virus and coordinate responses3.
These measures aim to educate the public, protect vulnerable populations, and prevent the spread of monkeypox.
Countering panic and educating the public about monkeypox involves clear communication, community engagement, and practical guidance. Here are some strategies to achieve this:
Countering Panic
- Accurate Information: Provide clear, accurate, and up-to-date information about monkeypox, its symptoms, transmission, and prevention1. Misinformation can lead to unnecessary fear.
- Transparency: Be transparent about the situation, including the number of cases, recovery rates, and measures being taken to control the outbreak1.
- Reassurance: Emphasize that monkeypox is less contagious than COVID-19 and that effective measures are in place to manage and contain the virus1.
Educational Measures
- Public Awareness Campaigns: Use various media platforms (TV, radio, social media) to disseminate information about monkeypox1.
- Community Engagement: Work with community leaders and organizations to spread awareness and educate people about preventive measures1.
- Workshops and Seminars: Organize educational sessions for the public, healthcare workers, and other stakeholders to provide detailed information about monkeypox1.
Preventive Measures at the Individual Level
- Vaccination: Encourage vaccination for those at high risk, such as healthcare workers and people in outbreak areas1.
- Hygiene Practices: Promote regular hand washing with soap and water or using alcohol-based hand sanitizers1.
- Avoid Close Contact: Refrain from close physical contact with individuals showing symptoms of monkeypox1.
- Protective Clothing: Use gloves and protective clothing when caring for infected individuals or handling animals1.
Preventive Measures at the Community Level
- Isolation and Quarantine: Isolate infected individuals and quarantine those who have been exposed to the virus1.
- Disinfection: Regularly clean and disinfect surfaces and materials that may have been contaminated1.
- Public Health Infrastructure: Strengthen public health infrastructure to ensure rapid response and effective management of outbreaks1.
Communication Strategies
- Clear Messaging: Use simple and clear language to explain preventive measures and the importance of following them1.
- Visual Aids: Utilize infographics, posters, and videos to make information more accessible and engaging1.
- Feedback Mechanisms: Establish channels for the public to ask questions and provide feedback, ensuring their concerns are addressed promptly1.
By implementing these strategies, we can effectively counter panic and educate the public about monkeypox, ensuring both individual and community safety.
If you enjoyed this article, please like and share it with your friends. Don’t forget to Share your personal experience/observations thoughts and valuable suggestions for the education /benefit of others. Do subscribe to remain onboard and get more great content!
Disclaimer: The contents of this article are intended to raise awareness about common health issues and should not be viewed as sound medical advice for your specific condition. You should always consult with a licensed medical practitioner before following any suggestions outlined in this article or adopting any treatment protocol based on the article’s contents.
Climate Change 2024:Unusual Catastrophic Weather Patterns in Pakistan