Moringa: The Miracle Tree of 2024
Understanding Heart Diseases: Guide to Cardiovascular Health in 2025
Understanding Heart Diseases: A Guide to Cardiovascular Health
Heart diseases, or cardiovascular diseases, affect millions worldwide. These conditions impact the heart and blood vessels, leading to significant health issues. Let’s delve into the common types of heart problems, their causes, symptoms, and treatment options.
Heart disease in the United States
In the United States:
- Heart disease is the leading cause of death for men, women, and people of most racial and ethnic groups.1
- One person dies every 33 seconds from cardiovascular disease.1
- In 2022, 702,880 people died from heart disease. That’s the equivalent of 1 in every 5 deaths.12
- Heart disease cost about $252.2 billion from 2019 to 2020.2 This includes the cost of health care services, medicines, and lost productivity due to death.
Common Types of Heart Diseases
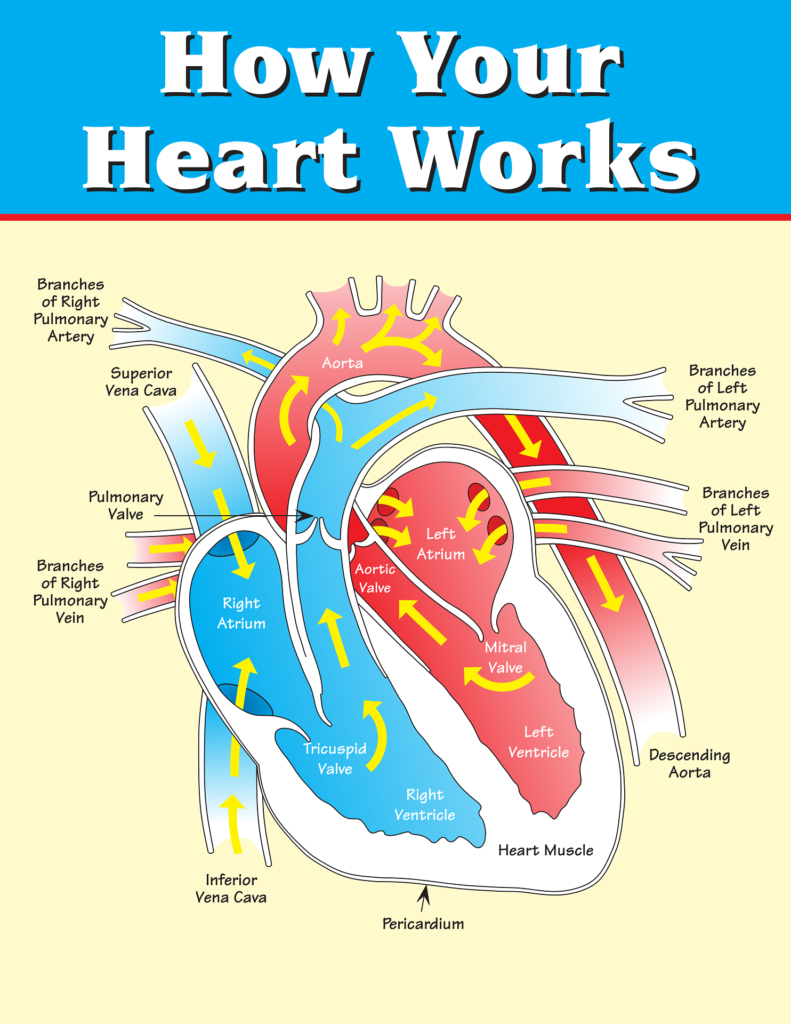
Coronary Artery Disease (CAD): When coronary arteries narrow or block due to plaque buildup, it can lead to chest pain (angina) or a heart attack.
Heart Failure occurs when the heart fails to pump blood effectively, causing shortness of breath, fatigue, and swelling in the legs and ankles.
Arrhythmias: Irregular heartbeats, such as atrial fibrillation (AFib), can increase the risk of stroke.
Heart Valve Problems: Valves may not open or close properly, forcing the heart to work harder and potentially leading to heart failure.
Aortic Aneurysm: The aorta, the major blood vessel, weakens and bulges, posing a serious health risk.
Causes and Risk Factors
Various factors for heart diseases
Genetics
High blood pressure
High cholesterol
Smoking
Obesity
Diabetes
Sedentary lifestyle
Diagnosing heart disease involves a combination of physical exams, medical history, and various tests. Here’s an overview of the process:
Initial Evaluation
Medical History: Your doctor will ask about your symptoms, family history, lifestyle, and any risk factors for heart disease.
Physical Exam: This includes checking your heart rate, blood pressure, and listening to your heart and lungs.
Diagnostic Tests
Blood Tests: These can check for levels of certain fats, cholesterol, sugar, and proteins that indicate heart disease.
Electrocardiogram (ECG or EKG): This test records the electrical activity of the heart and can detect irregularities in heart rhythm, heart attacks, and other conditions.
Echocardiogram: Uses sound waves to create images of the heart, showing its structure and function.
Stress Test: Measures how your heart and blood vessels respond to exertion, often involving walking on a treadmill or riding a stationary bike.
Holter Monitoring: A portable ECG device is worn for 24-48 hours to monitor heart activity over time.
Cardiac Catheterisation: Involves inserting a catheter into a blood vessel to reach the heart, allowing for detailed imaging and measurement of blood flow and pressure.
CT Scan or MRI: These imaging tests provide detailed pictures of the heart and blood vessels, helping to identify blockages or other issues.
Symptoms to Watch For
Chest Pain or Discomfort: Often described as pressure, tightness, or squeezing in the chest.
Shortness of Breath: Especially during physical activity or when lying down.
Fatigue: Unexplained or extreme tiredness.
Swelling: In the legs, ankles, or abdomen.
Irregular Heartbeat: Palpitations or a fluttering sensation in the chest.
If you experience any of these symptoms or have concerns about your heart health, it’s important to consult with a healthcare professional for a thorough evaluation and appropriate testing.
If you suspect you are having a heart attack, it’s crucial to act immediately. Here’s what you should do:
Immediate Steps
Call Emergency Services: Dial 911 or your local emergency number right away. Don’t wait.
Chew Aspirin: If you have aspirin available and are not allergic, chew one regular-strength aspirin (325 mg). This helps to prevent blood clotting.
Stay Calm and Sit Down: Try to remain as calm as possible. Sit down and rest while waiting for emergency responders.
Take Nitroglycerin: If you have been prescribed nitroglycerin for heart problems, take it as directed.
Avoid Physical Activity: Do not exert yourself. Rest and wait for help to arrive.
Recognizing Symptoms
Be aware of the symptoms of a heart attack:
Chest pain or discomfort, often described as pressure, squeezing, or fullness
Pain or discomfort in the arms, neck, jaw, back, or stomach
Shortness of breath
Cold sweat
Nausea or vomiting
Lightheadedness or dizziness
In case of a heart attack, it’s crucial to act quickly. Here are the steps to follow:
Call Emergency Services: Dial 911 or your local emergency number immediately. Don’t delay this step.
Stay Calm: Keep the person calm and reassure them that help is on the way.
Take Aspirin: If the person is not allergic and it’s recommended by emergency services, have them chew a regular-strength aspirin (325 mg) to help prevent blood clotting.
Administer Nitroglycerin: If the person has a prescription for nitroglycerin, help them take it as directed.
 Start CPR: If the person is unresponsive and not breathing, begin CPR:
Start CPR: If the person is unresponsive and not breathing, begin CPR:
Place your hands in the centre of the chest, between the nipples.
Push hard and fast, at a rate of 100-120 compressions per minute.
Continue until emergency responders arrive or the person starts to breathe again.
Use an AED: If an Automated External Defibrillator (AED) is available, use it as soon as possible. Follow the device’s instructions carefully.
Remember, time is critical in a heart attack situation. Acting quickly can save a life.
Prevention and Treatment
Early detection and treatment are crucial. Lifestyle changes like a healthy diet, regular exercise, and quitting smoking can make a significant difference. Some cases may require medication or surgery.
Heart Attack vs. Cardiac Arrest
Understanding the difference between a heart attack and cardiac arrest is vital.
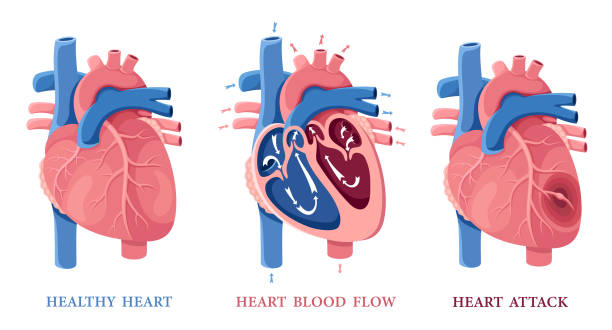
Heart Attack: A blockage prevents oxygen-rich blood from reaching part of the heart muscle, causing damage. Symptoms include chest pain, shortness of breath, and pain in the arms, neck, jaw, or stomach.
Cardiac Arrest: The heart suddenly stops beating effectively, leading to unconsciousness and no breathing. Immediate treatment with CPR and defibrillation is necessary.
It’s important to note that a heart attack can lead to cardiac arrest, but not all cardiac arrests are caused by a heart attack.
Symptoms of Heart Attack and Cardiac Arrest
Heart Attack Symptoms:
Chest pain or discomfort
Shortness of breath
Pain in arms, neck, jaw, or stomach
Sweating
Nausea or vomiting
Lightheadedness or dizziness
Cardiac Arrest Symptoms:
Sudden collapse
Loss of consciousness
No pulse or breathing
Agonal breathing (gasping)
Electrolyte Imbalance and Its Impact
Electrolyte imbalance occurs when the levels of electrolytes in the body are too high or too low. Key electrolytes include sodium, potassium, chloride, and calcium.
Causes of Electrolyte Imbalance:
Dehydration from sweating, vomiting, or diarrhoea
Renal disorders, like chronic kidney disease
Medications, such as diuretics and laxatives
Hormonal imbalances, like Addison’s disease and hyperthyroidism
Symptoms of Electrolyte Imbalance:
Fatigue
Muscle weakness or cramping
Numbness or tingling
Irregular heartbeat
Confusion
Seizures
Treatment typically involves addressing the underlying cause and replenishing electrolytes through fluids, medications, or hospitalisation.
Sleep Apnea: Diagnosis and Risks:
Sleep apnea is a disorder that causes interruptions in breathing during sleep. There are three types:
Obstructive Sleep Apnea (OSA): Muscles in the throat fail to keep the airway open.
Central Sleep Apnea (CSA): The brain fails to send proper signals to the breathing muscles.
Complex Sleep Apnea Syndrome (Compsa): A combination of OSA and CSA.
Symptoms of Sleep Apnea:
Loud snoring
Choking or gasping during sleep
Insomnia
Daytime fatigue
Morning headache
Diagnosing Sleep Apnea
A healthcare professional may recommend a sleep study to diagnose sleep apnea. A polysomnogram (PSG) conducted in a sleep lab monitors brain waves, eye movements, heart rate, and breathing. Home sleep apnea testing (HSAT) is another option for measuring airflow and breathing patterns at home.
Early diagnosis and treatment can mitigate risks associated with sleep apnea, such as high blood pressure, heart attack, and stroke.
Understanding Sleep Apnea and Its Diagnosis
What is Sleep Apnea?
Sleep apnea is a sleep disorder where a person stops breathing for short periods during sleep. It is often mistaken for cardiac arrest or a heart attack. There are three main types of sleep apnea:
Obstructive Sleep Apnea (OSA): The most common type. It happens when the throat muscles fail to keep the airway open.
Central Sleep Apnea (CSA): Occurs when the brain doesn’t send proper signals to control breathing.
Complex Sleep Apnea Syndrome (CSA): A combination of OSA and CSA.
Symptoms of Sleep Apnea
Loud snoring
Choking or gasping during sleep
Insomnia
Daytime fatigue
Morning headache
Sleep apnea increases the risk of high blood pressure, heart attack, stroke, and other health problems.
Diagnosing Sleep Apnea
A healthcare professional will conduct a physical exam, review your medical history, and discuss your symptoms. They may recommend a sleep study, which can be done in a sleep laboratory or at home.
Polysomnogram (PSG): An overnight test in a sleep lab, monitoring brain waves, eye movements, heart rate, and breathing.
Home Sleep Apnea Testing (HSAT): Measures airflow and breathing patterns at home.
Based on the sleep study results, the healthcare professional can diagnose sleep apnea and determine the appropriate treatment.
How to Treat Sleep Apnea
Treatment for sleep apnea usually involves lifestyle changes and medical therapy to keep the airway open during sleep. Common treatments include:
Continuous Positive Airway Pressure (CPAP): A mask over the nose or mouth delivers a steady stream of air to keep the airway open.
Oral Appliances: Worn in the mouth during sleep to keep the airway open, recommended for mild to moderate OSA.
Surgery: In some cases, surgery may be necessary to remove excess tissue or repair structural abnormalities.
Lifestyle Changes: Losing weight, avoiding alcohol and sedatives, and sleeping on your side can reduce the severity of sleep apnea.
Behavioural Therapy: Changes behaviour to improve sleep, such as avoiding caffeine and nicotine, maintaining a regular sleep schedule, and avoiding daytime naps.
Adaptive Servo-Ventilation (ASV): Similar to CPAP, but uses an advanced algorithm to adjust air pressure based on breathing patterns.
The best treatment depends on the severity of your sleep apnea, overall health, and personal preferences. Regular follow-ups with your healthcare provider are essential to evaluate the treatment’s effectiveness and make necessary adjustments. Understanding sleep apnea and its diagnosis is crucial for managing the condition and preventing complications. By recognising symptoms and seeking appropriate treatment, individuals can significantly improve their quality of life.
Lesser-Known Heart-Related Complications
Many people are unaware of certain heart-related conditions. These include:
Heart Arrhythmias: Irregular heart rhythms like atrial fibrillation (AFib) or ventricular tachycardia (VT), which increase stroke or heart failure risk.
Heart Valve Problems: Conditions like aortic stenosis or mitral regurgitation can lead to heart failure.
Cardiomyopathy: Affects the heart muscle’s structure and function, making it harder to pump blood.
Pulmonary Hypertension: High blood pressure in the lungs, which strains the heart.
Pericarditis: Inflammation of the sac surrounding the heart.
Aortic Dissection: A tear in the inner layer of the aorta, a serious condition.
Coronary Microvascular Disease (MVD): Affects small vessels in the heart, is common in women, causing chest pain and heart attack.
Heart Murmurs: What You Should Know
A heart murmur is an abnormal sound during a heartbeat, caused by turbulent blood flow. They can result from:
Heart Valve Problems: Stenosis (narrowing) or regurgitation (leakage).
Heart Muscle Disorders: Such as cardiomyopathy.
Blood Flow Problems: Like aortic stenosis.
Congenital Heart Defects: Such as holes in the heart.
Not all heart murmurs are serious; some are benign (innocent murmurs). A healthcare professional will diagnose a heart murmur by listening to the heart with a stethoscope and may perform other tests like an echocardiogram (ECG) or cardiac catheterisation.
Gender Differences in Heart Disease
Heart disease affects both men and women, but there are some differences:
Symptoms: Men often have classic heart attack symptoms like chest pain, while women may experience atypical symptoms like shortness of breath, fatigue, or stomach pain.
Risk Factors: High blood pressure, high cholesterol, and smoking affect both genders. However, women face a higher heart disease post-menopause due to decreased estrogen levels.
Coronary Microvascular Disease (MVD): More common in women, causing chest pain and heart attacks.
Heart Failure: Men and women have similar rates but different causes. Men often suffer from heart attacks or blocked arteries, while women are more likely to have high blood pressure-related heart failure.
Treatment: Generally the same, but women may be less likely to receive invasive procedures like angioplasty or bypass surgery.
Both men and women should be aware of their heart disease risk and take steps to reduce it, such as maintaining a healthy lifestyle, managing chronic conditions, and seeking medical care when needed.
When Open Heart Surgery, Stent Insertion, and Bypass Surgery Become Mandatory
Open Heart Surgery
Open heart surgery is a major procedure performed under general anaesthesia. It involves opening the chest to access the heart for repair or replacement of damaged heart valves or vessels. It is typically recommended for:
Severe heart valve problems
Significant heart muscle damage from a heart attack
Stent Insertion
Stent insertion is less invasive than open-heart surgery. It is used to open blocked or narrowed coronary arteries. The procedure involves threading a catheter through a blood vessel in the arm or leg to the blocked artery, where a stent (tiny mesh tube) is placed to improve blood flow to the heart.
Bypass Surgery
Bypass surgery redirects blood flow around a blocked or narrowed coronary artery. It involves using a blood vessel from another part of the body to create a new pathway for blood to reach the heart muscle. It is recommended for:
Severe blockages in multiple coronary arteries
Non-Surgical Options Before Surgery
Surgery is often a last resort. Doctors typically try several non-surgical options first:
Lifestyle Changes
Diet and exercise improvements
Weight loss
Quitting smoking
Stress management
Medications:
Blood pressure-lowering medications
Cholesterol-lowering medications
Blood thinners
Angioplasty and Atherectomy
These procedures open blocked or narrowed coronary arteries using a catheter to widen the artery or remove plaque.
Ablation
This procedure destroys or removes small areas of heart tissue, causing abnormal electrical signals, used to treat arrhythmias like atrial fibrillation.
Heart Assist Devices
Devices like ventricular assist devices (VAD) or total artificial hearts (TAH) help the heart pump blood until a transplant can be performed.
An overview of recent advancements and preventive measures in healthcare:
Latest Technology Inventions for Heart Disease/ Complications and Medicines
Artificial Intelligence (AI): AI is revolutionising healthcare by improving early disease detection and diagnosis. For example, AI algorithms can analyse mammograms 30 times faster with almost 100% accuracy, reducing the need for biopsies.
3d Printing: This technology is being used to create dental implants, replacement joints, and prosthetics. Research is also underway to use 3d printers for manufacturing skin tissue, organs, and even medication.
Minimally Invasive Procedures
New procedures with smaller incisions, faster recovery times, and less pain. Examples include:
Transcatheter Aortic Valve Replacement (TAVR)
Atrial Fibrillation Ablation
Robotic Surgery
Robotic technology is used in heart surgery for more precise and accurate procedures, such as mitral valve repair.
Heart Monitoring Devices
Wearable devices continuously monitor heart rate, blood pressure, and other vital signs to help manage symptoms and track progress.
Stem Cell Therapy
Researchers are exploring stem cell therapy to repair or regenerate damaged heart tissue, offering potential alternative treatments for heart failure.
CRISPR Gene Editing: This groundbreaking technology allows for precise editing of DNA, which can potentially cure genetic disorders.
Virtual Reality (VR): VR is being used for pain management, rehabilitation, and even surgical training.
Smart Bandages: These bandages can monitor wounds and deliver medication as needed, improving healing times and reducing infection risks.
New Medicines:
Zilebesiran: This investigational medication decreases the body’s production of angiotensinogen, a protein that plays a key role in increasing blood pressure. It has shown promising results in reducing blood pressure.
Acoramidis: A new drug for transthyretin amyloid cardiomyopathy (ATTR-CM), which stabilises the transthyretin protein to prevent amyloid formation. It has shown significant benefits in terms of mortality, morbidity, and physical function.
SGLT-2 Inhibitors: These diabetes drugs have been found to help people with heart failure by reducing complications, preventing hospitalisations, and improving survival rates.
Preventive Measures:
Healthy Diet and Exercise: Maintaining a balanced diet and regular physical activity are crucial for heart health.
Regular Check-ups: Routine health screenings can help detect issues early and manage them effectively.
Smoking Cessation: Quitting smoking significantly reduces the risk of heart disease.
Stress Management: Techniques like meditation, yoga, and mindfulness can help reduce stress, which is a major risk factor for heart disease.
Vaccinations: Staying up-to-date with vaccinations can prevent illnesses that may exacerbate heart conditions.
Choosing the best treatment depends on the individual’s condition and overall health. Doctors work with patients to determine the most appropriate options. Regular check-ups and follow-ups are crucial to evaluate treatment effectiveness and make necessary adjustments.
Conclusion
Heart disease and related conditions like electrolyte imbalance and sleep apnea are serious health issues that require prompt attention and care. Understanding these conditions, recognising symptoms, and seeking early treatment can significantly improve outcomes.
References:
World Health Organisation (WHO)
American Heart Association (AHA)
National Heart, Lung, and Blood Institute (NHLBI)
Disclaimer: The contents of this article are intended to raise awareness about common health issues and should not be viewed as sound medical advice for your specific condition. You should always consult with a licensed medical practitioner before following any suggestions outlined in this article or adopting any treatment protocol based on the contents of this article.
If u understand this article, please like and share it with your friends. Don’t forget to share your personal experience/observations, thoughts and valuable suggestions for the education /benefit of others. Do subscribe to remain onboard and get more great content!
Heart-Healthy Lifestyle, Healthy Habits for a Strong Heart in 24/25